Patients with neurogenic OAB tend to have severe symptoms that are more difficult to treat pharmacologically. It is not immediately clear that the overactive contractions experienced by patients with neurological conditions are necessarily of greater amplitude or occur earlier during filling, although there is some indirect evidence to support this contention (13). Phasic detrusor contractions that crescendo and result in urge-related urine leakage appear to be more commonplace in patients with neurogenic overactivity, for example, in patients with multiple sclerosis (MS) (Fig. 6). Voiding dysfunction, either with or without DO, also appears to be common in patients with MS. True detrusor external sphincter dyssynergia may be present in many as 40% of patients with LUTS secondary to MS (20); the incidence of bladder neck dyssynergia independent of detrusor overactivity may be even higher.
Patients with movement disorders also appear largely to suffer from DO on urodynamic testing. One unique finding among patients with movement disorders involves external sphincteric testing. Incompetent external sphincteric function resulting from denervation secondary to neuronal cell loss in the anterior horn of Onuf’s nucleus is present in the majority of patients with multiple system atrophy and can lead to debilitating urinary incontinence (21).
Both sphincteric deficiency and sphincteric bradykinesia (failure to relax) have been described in patients with PD, making surgical endeavors to treat BOO presumed secondary to prostatic obstruction treacherous because incontinence rates following transurethral prostatectomy among patients with PD have historically ranged as high as 20%. It is unclear whether this dismal rate of success will be improved with other heat-based prostatic treatments.
Patients with interruptions of the spino-bulbo-spinal pathway, typically as a result of spinal cord injury, may have debilitating urinary incontinence in addition to severely impaired bladder emptying secondary to detrusor external sphincter dyssynergia (Fig. 7).
 Fig. 6. Phasic detrusor overactivity (closed arrows) resulting in urinary leakage (open arrows) in patient with multiple sclerosis and urge incontinence.
Fig. 6. Phasic detrusor overactivity (closed arrows) resulting in urinary leakage (open arrows) in patient with multiple sclerosis and urge incontinence.
{embed=“ref/stat-menu-urodynamic-assessment”}
In these instances, detrusor pressures may remain elevated because of the sustained detrusor contraction (particularly true in spinal cord injury) in the absence of external sphincter, and frequently bladder neck, relaxation. Concurrent fluoroscopic monitoring can be useful to evaluate for bladder wall abnormalities or vesicoureteral reflux and further evaluate sphincteric function. In patients with severe or detrusor dysfunction, bladder diverticula can develop (Fig. 8), which can ultimately result in further impairment of bladder drainage and create a haven for the development of bladder stones and malignant bladder lesions.
Conclusion
Urodynamic testing remains an integral part of the complete evaluation of patients with OAB symptoms, particularly those who fail to respond to conventional management strategies, those with specific complaints of voiding dysfunction, and those with neurogenic bladder disease.
 Fig. 7. Detrusor sphincter dyssynergia in patient with T5 spinal cord injury. Note sustained intravesical pressure elevation (closed arrow) and simultaneous sphincteric activity (open arrow).
Fig. 7. Detrusor sphincter dyssynergia in patient with T5 spinal cord injury. Note sustained intravesical pressure elevation (closed arrow) and simultaneous sphincteric activity (open arrow).
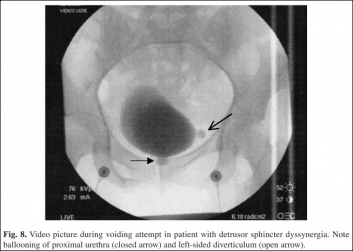 Fig. 8. Video picture during voiding attempt in patient with detrusor sphincter dyssynergia. Note ballooning of proximal urethra (closed arrow) and left-sided diverticulum (open arrow).
Fig. 8. Video picture during voiding attempt in patient with detrusor sphincter dyssynergia. Note ballooning of proximal urethra (closed arrow) and left-sided diverticulum (open arrow).
Although the urological community continues to search for less-invasive means of monitoring bladder function, at the present time multichannel urodynamic testing is the most accurate and reliable assessment tool, and it provides a means of directing appropriate therapeutic strategies, determining treatment response, and monitoring for disease progression.
——
Gary E. Lemack, MD
——
{embed=“ref/3”}